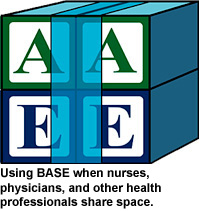
Four blocks in this photo help explain what nurses do, but which ones?

We sat in the corner of a noisy coffee shop in deep dialogue. I came at the invitation of this physician, a retired chief executive officer of a major healthcare system. He was writing a piece about interprofessional practice and wanted better understanding of the unique contribution of nurses.
 “So, Teddie, you have succinctly told me what physicians do on the team. We diagnose and treat. What do nurses offer? Tell me in one or two words what you do.”
“So, Teddie, you have succinctly told me what physicians do on the team. We diagnose and treat. What do nurses offer? Tell me in one or two words what you do.”
Could you tell him in one or two words what nurses do? I couldn’t, so I answered with a question: “Imagine you have a medically fragile patient in the hospital. You have correctly diagnosed the condition and ordered the appropriate medications. If nurses weren’t present, what would happen to your patient?”
The physician thought for a while and then said, “He’d die.” I looked him in the eye and responded, “And that is what nurses do.”
As nurses, we frequently struggle to explain what we do and why our presence is so vitally important. However, until we are able to explain our unique contribution, we will be overlooked, undervalued, and either not invited to or not taken seriously at the interprofessional table. It is not the role of others to define us. We need to clearly state and proudly claim our unique medicine or contribution to healing.
What makes this so difficult for nurses to do? There are many contributing factors, including historical patterns of oppression both internal and external to the profession, nursing curricula that is overly focused on the medical model to the detriment of nursing’s unique science, social hierarchies within the profession where one nursing role is thought to be more important than others, and, quite frankly, lack of vision and confidence that we have the right to be full partners in redesigning healthcare. I am focusing here on shifting the nursing paradigm so we can be a powerful and unified voice at the interprofessional table. If you want to talk about the other issues, invite me for a cup of coffee!
In my first course as an undergraduate nursing student, I learned a paradigm that includes humans, health, the environment, and nursing practice. I failed to gain clarity, however, about how these concepts relate. We spent very little time talking about what nurses have in common with one another before we plunged into specialized medical-surgical knowledge. I did not learn how to succinctly tell others who nurses are and what we do. I did not leave school able to clearly articulate what would happen in a world without nurses.
 It took 3 1/2 decades of caring for patients and families and teaching nurses before I was finally able to define nursing. I developed a unifying paradigm called the BASE of Nursing Practice (Eisler & Potter, 2014). Designed to be used by all nurses in all roles and in all locations, it illuminates nursing’s unique medicine and contribution to healing and ensures nursing’s full partnership and participation in interprofessional collaborative practice.
It took 3 1/2 decades of caring for patients and families and teaching nurses before I was finally able to define nursing. I developed a unifying paradigm called the BASE of Nursing Practice (Eisler & Potter, 2014). Designed to be used by all nurses in all roles and in all locations, it illuminates nursing’s unique medicine and contribution to healing and ensures nursing’s full partnership and participation in interprofessional collaborative practice.

 Four domains
Four domains
The BASE of Nursing Practice paradigm includes four domains of equal importance. The four domains are:
- Being present
- Active caring
- Stories or evidence from narratives
- Evidence from science
Nurses need to be proficient in all domains, applying them fully in practice, research, and teaching. If any one of the domains is missing, the full potential of nursing is compromised.
The BASE of Nursing Practice paradigm acknowledges two ways of being: 1) being present with those in need and 2) active caring through nursing interventions.
The BASE of Nursing Practice model also recognizes two ways of knowing: 1) knowledge originating from stories told by patients and families, and 2) knowledge originating from the science of nursing, healthcare, and other fields of inquiry.
 Being present
Being present
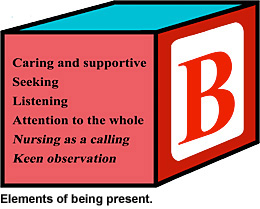
Being present can also be known as “therapeutic use of the self.” It involves awareness of space and proximity to those needing nursing care. Being present requires intentional use of body, voice, and time. Elements of being present are shown at right.
When nurses practice true presence, they enter a state where deep interconnection with those they serve becomes possible. Those who regularly practice being present may feel as though time stands still.
 Active caring
Active caring
Through being present, nurses earn the trust of patients, families, and communities and, therefore, are privileged to hear their stories. These stories point us in the right direction to find the most effective scientific evidence to guide our practice. Once we know the best practice, we can act with care.
Active caring takes many different approaches. Whether it’s doing skilled interventions or creating effective healthcare policies, nurses are not simply caring professionals; nurses are professionals who put care into action. Examples of active caring are shown below.
 Stories: Narrative-based evidence
Stories: Narrative-based evidence
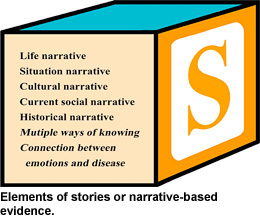
Nurses are taught to collect data but rarely are urged to collect stories. Stories hold the key to healing and, therefore, occupy an essential domain in the nursing paradigm. Stories are subjective. They reveal the meaning that a wellness or illness event has for a patient, family, or even a community. Stories are only told when there is a safe and supportive relationship, when the person telling the story feels there is time to do so, and when they feel the person listening is totally present. Stories often come out just as nurses are preparing to leave. Frequently, they begin with, “You may not need to know this but …”
Here are some examples:
- “You may not need to know this, but I fell in the bathroom last night. I didn’t tell the doctor because I am afraid, and I want to go home.”
- “You might not need to know this, but I don’t take the medications I am prescribed because I don’t have money for the co-pays, and I feel ashamed.”
- “You might not need to know this, but I am terrified about tomorrow’s surgery because my dad died when he had the same procedure 30 years ago.”
- “You might not need to know this, but I am afraid to go home. When my boyfriend drinks, I can’t seem to do anything right. I know he doesn’t mean to, but he has hit me now and then.”
I have come to recognize the unique feel or energy of a story. When it starts, I turn my full attention to the story being told as though nothing else in the world matters, for, in fact, nothing else does matter. The story reveals what a particular person, family, or community needs to heal. Some elements of stories—narrative-based evidence—are shown below.
Solutions to what people need to heal are often embedded in the stories they tell. If we fail to listen to a story, our tendency will be to offer another pill or a standardized intervention. No wonder healthcare costs are rising and patient satisfaction is declining. Too frequently we fail to listen—to truly listen—to the story. Stories accurately point us in the direction of the most effective evidence-based practices.
Evidence from science
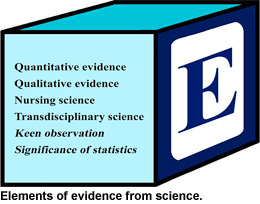 Once the nurse knows the patient, family, or community narrative, best-practice guidelines can be sought from science. Drawing from information contained in a story, the nurse can then consult best practices for:
Once the nurse knows the patient, family, or community narrative, best-practice guidelines can be sought from science. Drawing from information contained in a story, the nurse can then consult best practices for:
- Creating a safe discharge plan for patients with a fall risk
- Assisting patients with information about paying for treatments
- Providing preoperative emotional support
- Protecting patients from domestic abuse
Applying the four domains
The BASE of Nursing Practice paradigm can be applied in every role and practice setting. It can be used to nurse patients, families, communities, organizations, or nations. It can inform nursing practice from urgent care to long-term care, from pediatric care to elder care, from the bedside to the boardroom. All nursing requires being present, receiving and honoring stories, using stories, and using current best practices to actively care. These are nursing’s ways of being and nursing’s ways of knowing.
To be full partners in
interprofessional practice, it is essential for nurses to recognize nursing’s unique contribution. This can be challenging because many things nurses know and do overlap with knowledge and action of many other health professionals. For example, I can insert an intravenous catheter. So can physicians. I can use evidence from The Lancet to guide my practice. So can physicians. This shared space may lead some people outside the profession to falsely assume that nurses are merely “step-down” physicians or physician helpers. Nothing could be further from the truth.
The unique medicine of nursing
If medicine is the art of healing and healing means to “make whole,” what is the medicine of nursing? How do we make people whole? What unique contribution do we bring to the interprofessional table? The answer resides in two of nursing’s domains. Nurses are present, and, through that presence, nurses hear the narratives of patients, families, and communities.
Nurses need to be prepared to respond, however, when physicians and other health professionals say, “I am present, and I listen to stories, too.” When I hear physicians make that claim, this is my response:
It may be confusing, because our professions have many similarities. We both care about the patients, families, and communities we serve, and we both respect and use the best current science to guide our practice.
You may want to be present, but the structure of healthcare today often prohibits you from spending the time required to be fully present. You may think you hear stories, but your education and responsibilities call you to focus on quantitative and qualitative data. There is nothing wrong with this. You are an expert diagnostician and prescribe effective treatments. I, on the other hand, am a nurse. My expertise is being present to hear the unique narratives of patients, families, and communities so I have a better understanding of what they need to heal.
Through interprofessional practice, we become greater than the sum of our parts. Working in partnership with patients, families, and communities, we are able to co-create effective plans to promote healing and maintain wellness.
Interprofessional practice requires nurses to know their unique medicine and be able to confidently state their contribution to healthcare. Unlike other professions whose “medicine” is standardized, the medicine of nursing is always consult best practices founique. Nurses are uniquely present for each patient, family, and community, and because we are fully present, we hear the unique narratives that are so important for effective and meaningful healthcare.
 In conclusion, my two words
In conclusion, my two words
Returning to the conversation I had with the physician at the coffee shop. When he asked, “What do nurses offer? Tell me in one or two words what you do,” I could have responded with certainty and confidence, “Nursing is
being and
knowing.”
Teddie M. Potter, PhD, RN, FAAN, clinical associate professor at the University of Minnesota School of Nursing, is coordinator of the school’s Doctor of Nursing Practice in Health Innovation and Leadership program, as well as director of inclusivity and diversity. She is executive editor for the Interdisciplinary Journal of Partnership Studies.
Reference:
Eisler, R., & Potter, T. (2014).
Transforming interprofessional partnerships: A new framework for nursing and partnership-based health care. Indianapolis, IN: Sigma Theta Tau International.