This chapter from High Reliability Organizations: A Healthcare Handbook for Patient Safety & Quality examines current demands for a highly reliable healthcare delivery system—a culture of quality and patient safety that anticipates risks and manages unexpected events.
"The biggest challenge we have in healthcare is not just to find the few holes that are really still there after years and decades of work, but it is to deal with layers of deficiencies that are more like sieves than they are shields."
—Dr. Mark R. Chassin
 In the United States, the healthcare industry has shifted from a mostly provider-controlled culture to a consumer-driven model. This has revealed the need to raise the bar on both quality and patient safety—in other words, on reliability. In healthcare, reliability means delivering failure-free health-related processes, procedures, or services in the required time. In this context, failure can result from not applying the appropriate evidence-based practice, failing to respond in a timely manner, or failing to practice patient-centeredness by including patient preference (Nolan, Resar, Haraden, and Griffin, 2004).
In the United States, the healthcare industry has shifted from a mostly provider-controlled culture to a consumer-driven model. This has revealed the need to raise the bar on both quality and patient safety—in other words, on reliability. In healthcare, reliability means delivering failure-free health-related processes, procedures, or services in the required time. In this context, failure can result from not applying the appropriate evidence-based practice, failing to respond in a timely manner, or failing to practice patient-centeredness by including patient preference (Nolan, Resar, Haraden, and Griffin, 2004).
Because of the complex, fragmented, and imbalanced healthcare system in the United States, the nation’s healthcare industry is struggling with how to respond to the growing demands of the government, private payers, and consumers. Each of these parties needs to see the value of each dollar that is spent.
In addition, under the Affordable Care Act (ACA) (U.S. Department of Health and Human Services, 2014), health insurance exchanges now give patients the option to shop for and compare health plans. This has made patients more conscious and aware of the service and quality of care they receive. As a result of these shifts, demands on the healthcare system to improve value, accessibility, efficiency, cost, service, and quality are growing. These issues are causing tremendous strain, stress, and safety risks among healthcare organizations and systems. There is pressure on all fronts for organizations to identify sustainable strategies to meet the needs of consumers and create a more reliable healthcare system. Clearly, a paradigm shift in healthcare is in order.
The purpose of this chapter is to discuss the current drivers of healthcare and the current healthcare culture. In addition, this chapter discusses why the high reliability organization (HRO) framework is a viable solution to addressing the complexity of the healthcare system.
Current drivers: Cost, cost, and cost
The U.S. healthcare system is in a state of flux. Many forces play a role in how the healthcare system is viewed as a whole. In addition, there is growing pressure to approach the delivery of healthcare differently. There is no doubt that the gap between the actual cost of care and reimbursement is increasing. The cost of healthcare is growing at an alarming rate, and access to care continues to be a challenge for many.
The U.S. is viewed by many countries as a leading nation in the world—except in its fundamental approach to providing healthcare to its citizens. In the U.S., healthcare is one of many goods in a free-market economy that citizens are expected to provide for themselves (with the exception of emergency services and Medicare benefits for inpatient, hospice, and home health services) (Barton, 2009). Many barriers affect citizens’ access to health services and have a direct impact on healthcare expenditures and health outcomes.
The U.S. consumes a higher percentage of its gross domestic product (GDP) for healthcare—17%, which is more than any other developed country (Rice et al., 2014). According to the World Health Organization (WHO, 2015), the per-capita total expenditure for healthcare by U.S. citizens in 2012 was $8,895. In comparison, in Canada, which is similar in size to the U.S. (though with a smaller population) and on the same continent, citizens spend $4,676 per capita (World Health Organization, 2015).
The cost of healthcare in the U.S. has not only strained the federal government, it has also affected state governments and the private sector as well. New quarterly health spending estimates from the U.S. Census Bureau (2015) showed that first-quarter 2015 spending was 7.3% higher than the first quarter of 2014. The increased coverage of the Affordable Care Act may be the cause of the increased usage of physicians and outpatient services and higher spending in hospitals. Along with the overutilization of diagnostic tests and procedures, healthcare providers experience challenges in encouraging consumers to become active participants in their health.
Other factors affect healthcare spending, too. The growth of the elderly population, prescription drug charges, and the rising cost of caring for a segment of the population suffering from chronic diseases make up a large portion of healthcare spending. Prescription drugs represent approximately 11% of the overall U.S. healthcare expenditure—a number that is expected to climb due to the expansion of healthcare coverage (Schumock et al., 2014). Lastly, the failure to manage chronic diseases has become a crisis in the U.S. and is draining the healthcare system. The most common and costly, yet preventable, health problems are heart disease, stroke, cancer, diabetes, and obesity. These conditions cost close to $800 billion (Centers for Disease Control and Prevention, 2015). According to the CDC (2015), approximately half of Americans have one or more chronic health conditions. All these key areas can take a toll on the government’s and on private insurers’ bottom lines.
A highly reliable healthcare industry can aid in bending the cost curve. A highly reliable healthcare environment is unique in that it embraces the use of standardized processes and procedures to provide efficient and effective care.
A push for performance
Because of the enormous dollars spent on healthcare, and because quality outcomes are below the standards expected in a developed country, health insurance payers have begun to question the value their beneficiaries are receiving. Healthcare organizations are experiencing a shift away from fee-for-service to value-based payment models. Payment models such as pay-for-performance and at-risk models have become more common. An example of a pay-for-performance program is the Centers for Medicare and Medicaid Services (CMS) Value-Based Purchasing program (CMS, 2015a). This approach moves away from incentivizing solely for quantity and moves toward accountability for quality, efficiency, and cost management. Pay-for-performance models have defined measures and require data collection and public reporting. In an at-risk model, base payment is predicated on the estimated expected cost of care to treat a condition or patient population. Success is based on the ability to manage cost control and expenditures.
These new payment models are a step toward improving quality and services, but doing so does not come without challenges. One challenge is agreeing on how to define and measure quality in healthcare. How value is defined by CMS and other regulatory agencies does not always align with the definition used by physicians, healthcare organizations, and consumers. CMS and commercial payers view value-based payment as a solution to growing healthcare costs. However, there are conflicting views on what quality measures to use to achieve value and lower cost. Some private insurers follow the CMS lead, whereas others have developed their own measures (Birk, 2015). This misalignment has contributed to uncertainty and unpredictability in the healthcare delivery system, where the overwhelming cry from providers, payers, and consumers is for standardization, transparency, and consistency.
Another key driver that is shifting the culture of healthcare is consumers’ growing demand that the healthcare delivery system demonstrate value. More and more, consumers are evaluating the healthcare services they receive. They’re accessing public reporting quality measures to choose their health plans and healthcare facilities. In 2012, Keckly and Coughlin published their longitudinal study of consumers’ perceptions of the healthcare delivery system between 2008 and 2012. The study revealed that the healthcare system’s overall performance has increased. However, the system was seen as confusing, complex, costly, and wasteful. There was little confidence that the healthcare industry was prepared to deal with future care expenses. Consumers did have confidence in their primary care physicians, but not in hospitals or their health plans. The current state of healthcare has made little progress since 2012. Healthcare spending remains out of control, and the industry has made only small incremental gains on the quality front.
To summarize, one driver that is shifting the healthcare culture paradigm is the focus on healthcare quality. More and more, quality performance and expectations have moved to center stage. Public reporting of healthcare systems’ and hospitals’ quality performance is used by insurance payers, financial institutions, and consumers to make decisions about their healthcare and investment. Unfortunately, the added spotlight on quality performance has not reduced incidences of patient harm or deaths due to preventable harm events in healthcare systems and hospitals.
Many years have passed since the Institute of Medicine’s (IOM’s) report “To Err Is Human” (1999), which sparked the nation to reflect on the state of the healthcare delivery system. It called for action to change how healthcare was being delivered. Although many healthcare systems and hospitals have made tremendous changes that have resulted in improved quality of care and patient safety, as a whole, the healthcare system and hospitals continue to experience unstirring results in preventable harm adverse events (IOM, 2011). In the category of operations being performed on the wrong side of the patient’s body or at the wrong site altogether, there are 50 incidents per week. Fires continue to break out in operating rooms. Thousands of patients experience hospital-acquired conditions, and harmful errors occur every year. Deaths even occur as a result of safety alarms—which go off several hundred times per day—being silenced or turned off (The Joint Commission, 2015a). Undoubtedly, more work is needed to raise patient safety to the top of the list of concerns for healthcare systems and hospitals.
The foundation of a high reliability organization (HRO) is to improve patient safety and quality performance through preventative strategies, robust process improvement programs, and the engagement of staff to speak up on safety concerns and participate in developing strategies to mitigate risks (Chassin, 2012).
Healthcare reform
The history of healthcare reform in the U.S. dates back to 1965, when President Lyndon Johnson introduced legislation that enacted Medicare (LBJ Presidential Library, 2012). In the last decade, progress has been made in both affordability and accessibility to healthcare. On March 23, 2010, President Barack Obama signed the Patient Protection and Affordable Care Act (PPACA), colloquially known as Obamacare or the Affordable Care Act (ACA). On March 30, 2010, PPACA became law after it was amended by the Healthcare and Reconciliation Act of 2010 (U.S. Department of Health and Human Services, 2014). On June 28, 2012, 2 years after PPACA became law, the United States Supreme Court upheld the ACA. A key part of the ACA was an individual mandate to obtain health insurance or to pay a penalty (U.S. Department of Health and Human Services, 2014). Since the passage of PPACA, there has been an increase of 11 million U.S. citizens with healthcare coverage (Congressional Budget Office, 2015).
In addition to expanding healthcare insurance coverage, healthcare reform shifted the landscape and paradigm of healthcare from volume to value. This shift has placed pressure on providers—healthcare systems, hospitals, and leaders—to demonstrate quality and service (Wagner, 2014). For healthcare systems and hospitals to be successful in this new environment, they must take a different approach to quality and service.
Value-based purchasing
The financial structure of the U.S. healthcare system is far from universal. The government funds significant areas in healthcare to support the public health programs known as Medicare and Medicaid. The remainder of insurance purchasers are employers and private payers (CMS, 2011). Given the rising cost of care, the government and private purchasers of healthcare have become more involved in the process of paying for healthcare. These purchasing groups have begun to monitor and measure how their dollars are spent. They also have come to expect improved quality and better clinical outcomes and service. This is collectively known as value-based purchasing (VBP), which is a purchasing practice that aims to increase the value of a dollar spent on improving quality and managing expenditures (CMS, 2011).
In 2010, the VBP program was established as part of the ACA. The VBP is a way for CMS to hold healthcare systems and hospitals accountable and to incentivize the use of evidence-based practices. It aims to enhance the quality of care and health outcomes and to improve the experience of care and value to its Medicare beneficiaries across various care settings (CMS, 2011). Participating hospitals are paid not only for quantity of service, but inpatient service is paid based on quality of service. The VBP program is “funded by a 1.75% reduction from participating hospitals’ base operating diagnosis-related groups (DRG) payments” (CMS, 2015a). Distribution of funds is based on a Total Performance Score (TPS), which is made up of quality performance measures. The approved set of measures are grouped in specific quality domains (CMS, 2011). Over the past 3 years, the CMS has raised the bar in quality expectations (see Table 1.1). In fiscal year (FY) 2016, outcome measure will hold 40% of the weight of the total measures (CMS, 2015b).
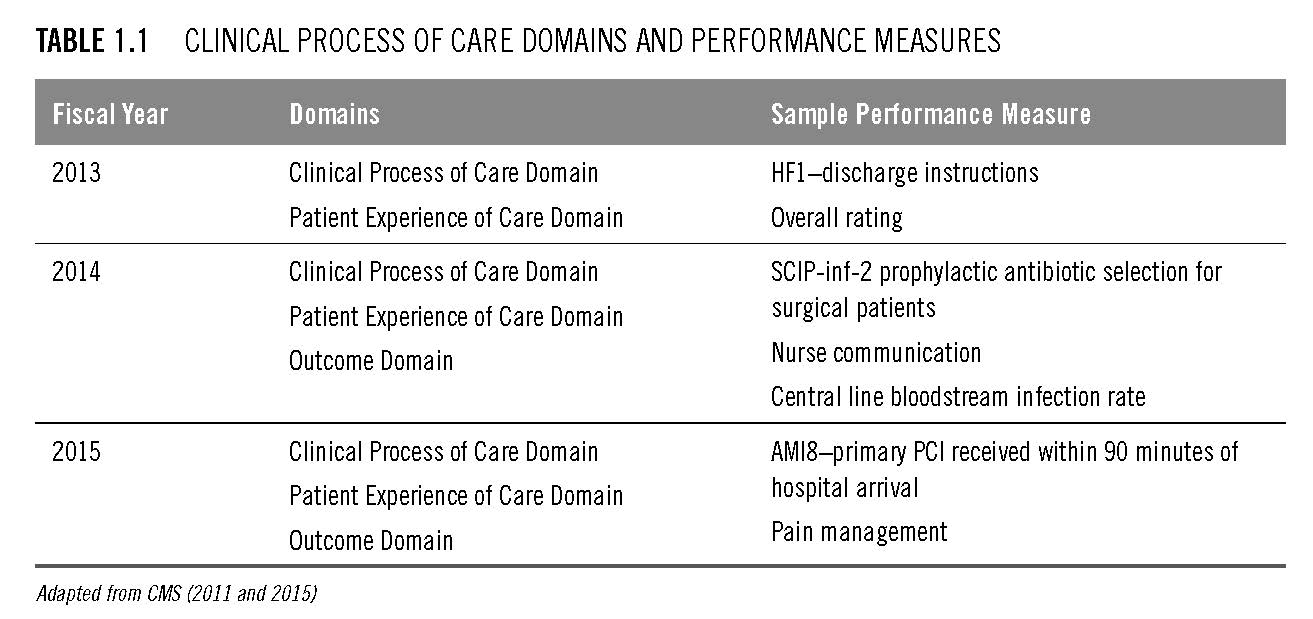
HROs view the measurement of performance as one of the key ingredients in evaluating the organization’s efficiency and effectiveness (Sutcliffe, 2011). The measurement of CMS VBP clinical and process metrics demonstrates measuring compliance with evidence-based practices and supports the essence of the HRO. Many of the CMS measures possess complex process steps and potential failure points, which cause patient safety issues and affect the organization financially.
Improving the quality of care in a healthcare organization requires focus on processes and outcomes. To achieve the expected measures, an organizational process must be reliable, providing the right care to the right patient at the right time. HRO principles encompass effective quality improvement tools that assist teams in eliminating waste and defects in a process. They also encompass robust analytics. Research demonstrates that healthcare organizations that use comprehensive process-improvement tools improve quality of care (DuPree et al., 2009; Chassin, 2015).
Healthcare regulation
Healthcare systems and hospitals are regulated by a broad range of regulatory bodies and programs from local, state, federal, and private organizations. All these agencies and programs set their own standards and measures. This can pose problems and sow confusion for those who provide care. Moreover, in some cases, the level of authority is not clearly defined. In addition to the federal regulatory bodies that provide oversight for healthcare systems and hospitals, physicians, and insurance companies are the coordinating bodies for the local and state agencies. On the private-sector side are organizations such as the American Medical Association and the Board of Nursing, which provide oversight of medical and nursing professionals, respectively. Supplemental government standards also exist, where the hospital industry can choose to supplement the state license through The Joint Commission (Field, 2008).
Despite these oversight challenges, the healthcare community, the private sector, and consumers would agree that regulatory agencies are essential to balancing the power of one agency over another. Also, these regulatory agencies aid in advocating for the safety of patients and employees in healthcare facilities and in holding providers, healthcare systems, and hospitals accountable for health outcomes. Founded in 1951, The Joint Commission is a leading not-for-profit organization that has certified more than 20,000 healthcare organizations and programs in the U.S. (The Joint Commission, 2015b). The Joint Commission’s mission is to “continuously improve healthcare for the public, in collaboration with other stakeholders, by evaluating healthcare organizations and inspiring them to excel in providing safe and effective care of the highest quality and value” (The Joint Commission Center for Transforming Healthcare, 2015). For hospitals to achieve accreditation from The Joint Commission, they must consistently meet many standards. Recently, The Joint Commission has added to these standards the accountability of hospital leadership to assess the hospital’s culture of safety. Collectively, only a relatively small percentage of health systems and hospitals across the country achieve top-quality honors from The Joint Commission. In 2014, approximately 36% of The Joint Commission–accredited hospitals were named “Top Performer on Key Quality Measured” (The Joint Commission, 2015b). Clearly, more than half the health systems and hospitals in the country have work to do in providing consistent care.
Although progress has been made in healthcare systems and hospitals, the chief medical officer of The Joint Commission, Ana Pujols McKee, states that there needs to be more focus on improvement processes and that building a high reliability safety culture is critical. Cultivating a culture of safety must start with senior leaders (Birk, 2015) of the healthcare system or hospital. Because of the incremental gains in safety improvement in hospitals as a result of the adoption of high reliability strategies and methodologies, The Joint Commission has become an advocate of the approach. The Joint Commission has developed a forum for best practices through the creation of The Joint Commission Center for Transforming Healthcare (Birk, 2015).
The HRO approach can help healthcare organizations design systems to aid in identifying unsafe conditions well before they lead to harm (Chassin, 2015). This is different from the current healthcare environment, which is more reactive to mistakes. Also, HROs recognize that all errors cannot be prevented and that safety can be derailed. In an HRO environment, there is a willingness to grant the team or individual the decision-making authority to address the safety risk.
Complexity
Depending on the field of study, complexity has various meanings. In healthcare systems, complexity is defined as the interrelatedness of components of a system. Complexity increases with the number of components, the number of relationships among them, and the uniqueness of these relationships (Kannampallil, Schauer, Cohen, and Patel, 2011). For instance, consider the difference in complexity between a community hospital and the Mayo Clinic health system. The Mayo Clinic has more components than a community hospital; therefore, it is more complex.
Complex systems create cognitive and physical challenges for internal and external individuals who interact with the system. Individuals internal to the system expend substantial cognitive effort in performing tasks or creating shortcuts. External users of the system are challenged with interacting with the system, and significant aspects of the system may be ignored (Kannampallil et al., 2011).
The current healthcare system has many components: hospitals, clinics, nursing homes, rehabilitation units, patient homes, patients, and families. These components add complexity for users and produce unintended consequences, such as adverse drug reactions, hospital-acquired infections, readmissions, and functional declines (Lipsitz, 2012). These complex issues make it difficult for an organization to achieve high reliability. Understanding the complexity of healthcare is central to improving quality and safety.
Serious events in healthcare organizations occur daily. These expose the failure of systems to provide a culture of safety for patients, staff, and providers as well as exposing ineffective communication. The complex nature of healthcare organizations contributes to myriad uncertainties that affect safety and quality of care. Teams that are well-versed in high reliability are more likely to address complex issues and recognize the most minor variance in expected outcomes (Wilson, Burke, Priest, and Salas, 2005).
Regulatory agencies are another layer of complexity that causes uncertainty and unpredictability for providers, caregivers, and healthcare leaders. With the conflicting views on quality and outcome measures, healthcare systems and hospitals are at risk of becoming complacent. The opposite can occur in hospitals that ignore warning signs to meet VBP and pay-for-performance measures (Lipsitz, 2012).
According to Lipsitz (2012), in complex systems, individual, self-organized behaviors naturally occur, such as the flocking of birds or the schooling of fish. This creates silos. The key to success is driving collective outcomes that are greater than the sum of their parts. However, this is difficult in the current health system due to silos and the lack of care coordination. Also, the fee-for-service payment model does not support this partnership. The 2013 IOM report, “Best Care at Lower Cost: The Path to Continuously Learning Health Care in America,” states that to achieve a high level of quality of care at a lower cost, there must be commitment across the system to learn from each other.
Current healthcare culture
Designing and sustaining a safety culture, which is required in order to improve reliability, is inherently difficult in healthcare due to the complexity. It is often difficult to visualize what is meant by safety. Patients add another level of complexity with regard to safety because human diseases are different from person to person. The design of the healthcare delivery process in itself creates safety risks and barriers, for which staff must implement workarounds (Khatri, Brown, and Hicks, 2009). Understanding the culture of healthcare and the various branches that add to the complexity can assist with developing solutions to address these challenges.
Many agree that the lack of a culture of safety in a healthcare organization could be a key contributor to organizational accidents. An organization’s culture can be viewed as what is valued, its beliefs, and the norms that determine how members interact and act toward patient care and safety. Dynamics of a safety culture can have a direct impact on how issues are detected, corrected, and understood. Therefore, organizations have begun to adopt mindfulness in their safety culture programs. The idea is that a higher level of mindfulness and individuals being more aware of their surroundings and actions can lead to fewer errors and incidents (Sutcliffe, 2011).
Building a culture of safety is essential in an HRO environment. Building a culture of safety requires the promotion of trust, reporting, and improvement. HROs balance learning and accountability through the implementation of a Just Culture, where discipline is equably applied across the system. There is a high sense of accountability with regard to adherence to safety measures and processes. Staff are expected to speak up when there is an error or problem. To learn from communication, there is a system to support ongoing feedback (Chassin, 2015).
Reactivity versus proactivity
The approach an organization takes for managing risk and preventing potential harm to patients depends on the organization’s approach to identifying and responding to patient safety issues. The approach used to manage and minimize risk varies from one healthcare system to another. More often than not, this approach is reactive rather than proactive. However, healthcare systems and hospitals should work to support a proactive approach to increasing patient safety and decreasing risk and exposure to liability. This is key in improving reliability.
When it comes to patient safety, what is the difference between being reactive and being proactive? A proactive approach involves an intentional effort to identify risks before events occur and to correct issues before they arise. A leader in a proactive organization takes ownership of identifying risks and causes of incidents instead of blaming circumstances, conditions, or conditioning. Such a leader’s behavior is the result of a conscious choice based on values, not feelings (Covey, 1989). This approach in preventing injury and loss allows for the ability to educate staff and the organization as a whole. In contrast, a reactive approach involves reviewing an event after it occurs for potential causes and process errors. With this approach, the patient could experience poor health outcomes as a result of the incident. This could lead to a legal claim (Stewart, 2011). A leader in this type of environment would more likely blame the event on circumstances or patient condition (Covey, 1989).
Suppose an elderly patient received a severe second-degree burn from a heating pad, which was used to treat back pain. In a reactive organization, the patient would receive treatment for the burn—possibly even a skin graft—and would face a long recovery. In a proactive organization, however, the staff would have been educated on the appropriate steps to take to apply the heating pad and the risk of burning to the elderly population, thereby preventing the incident in the first place.
It takes commitment, time, support, and an effective process-improvement program to develop a proactive organization. Once the program is in place, the organization’s learning capabilities and collaborative nature help to increase patient safety and decrease organizational exposure to liability (Stewart, 2011).
Blame/no blame to accountability
In managing risk, it’s important for an organization to have an understanding or philosophy of how providers, caregivers, and leaders are held accountable for their actions. It is human nature to demand answers for why an adverse event happens. There is often a strong need to blame someone for an error and hold that person accountable. With this approach, there is an assumption that the person chose to make the error instead of adopting a wrong procedure or process that was on hand at the time of the event. In 1999, Charles Perrow suggested that 60 to 80% of operating errors were in part a result of system errors or failures. In other words, the system—rather than a person—was at least in part to blame for the error. But most company leaders have found that a blaming culture does not foster an environment that brings safety issues to the surface. Organizations that pride themselves on creating a culture of safety routinely examine all aspects of the system after an adverse event. Applying a system approach to investigating an error or adverse event ensures there is no blame.
In healthcare that involves human activity and a reliance on technology, it is likely there could be a situation in which individuals experience a problematic interaction or conflict or incorrectly interpret the actions or words of another. It is also likely they will experience problems when interacting with technology.
HROs have transitioned from a culture of blame, in which an individual or group is seen as the reason for an error, to one that accepts that no organization is free from error and understands that identifying the cause of an error can both offer operational lessons and enhance organizational learning (Weick and Sutcliffe, 2001; Provera, Montefusco, and Canato, 2010). Blaming an individual or group can seriously hinder an organization’s ability to learn from the experience. In a blaming environment, individuals who make errors usually are not willing to share this information with their colleagues or managers. Instead, they try to fix it themselves or cover it up. The no-blame approach can be an effective way of enhancing an organization’s ability to learn.
Weick and Sutcliffe (2007) and Khatri, Brown, and Hicks (2009) describe a no-blame system as possessing several characteristics:
- Individuals are encouraged to report errors and near misses and are rewarded for doing so.
- A high level of trust and openness allows individuals to exchange opinions without feeling judgment.
- Purposeful organizational analysis takes place with individuals and groups who experience an error.
- Managers review and approve corrective action plans and communicate lessons learned throughout the organization.
- There is a learning culture, enabling healthcare organizations to elicit greater staff involvement.
- Human resources management is integrated in the performance-management process
Organizations that adopt a no-blame approach commit to a culture in which employees are mindful of their surroundings. Also, in this type of culture, employees become willing to support continuous organizational improvement and to make decisions to strengthen the organization (Weick and Sutcliffe, 2006). This can enable organizations to focus on the right things and avoid wasting valuable time.
When transitioning to a blameless culture, a spirit of accountability must play a role in managing human error. Many successful organizations have found that incorporating a disciplinary system that explores the role each person played in an event can foster an environment of organizational learning. In the healthcare industry, this approach is called a Just Culture (Center for Patient Safety, 2015). A Just Culture is characterized by a supportive environment in which the healthcare system or hospital holds itself accountable for the system it designs and holds providers and caregivers accountable for the choices they make within that system. Four behavioral concepts are used to evaluate discipline and patient safety:
- Human error
- Negligence
- Intentional rule violation
- Reckless behavior
In this type of environment, the individual is coached on his or her risky behavior, and the organization learns through the process.
Commercial airlines have led the way in adopting no-blame practices by developing an environment that promotes collaboration and respectful dialogue among pilots. The National Transportation Safety Board has removed the placement of blame from all events except in cases of criminal activity. Gathering information through various approaches—both formal and informal—is encouraged. Pilots and technicians are required to report any issues during operations, including their own errors. Investigations of errors are done systematically, and corrective measures are communicated to all personnel (Roberts, Bea, and Bartles, 2001).
High reliability organization theory
Organizational and human factors play a role in all accidents and incidents that result in patient harm. HRO theory focuses on the social and organizational foundation of system safety and accident prevention (Sutcliffe, 2011). Reliability is viewed as a top priority. HRO theory also suggests human processes and relationships are the underpinning of an HRO and a culture of safety (Weick and Sutcliffe, 1999). HROs that operate in high-risk environments or have high exposure to liability and loss demonstrate fewer errors than non-HROs. This is achieved through a driven passion for safety that is realized by the pursuit of two approaches (Sutcliffe, 2011):
- Prevention (anticipation): This involves an attempt to anticipate or identify risks that may lead to unplanned events or occurrences and to then create processes and procedures to avoid them. An example might be proactively shadowing a telemetry monitor technician to observe the application of a telemetry box to a patient and the implementation of continuous monitoring. This example might also involve identifying potential risks of failures in processes to ensure the right patient is connected to the right telemetry box.
- Resilience (containment): HRO cannot be achieved by prevention alone. It also requires resilience (Wildavsky, 1988). The essence of resilience is the ability to maintain or regain a stable state in the presence of stress. Resilience involves three abilities. First is the ability to absorb strain and preserve function in spite of adversity. Second is the ability to bounce back from untoward events. Third is the ability to learn and grow from previous episodes of resilient action (Sutcliffe, 2011). An example of resiliency is the heparin medication error that occurred in a California hospital in 2007. Three infants received 1,000 times more heparin than intended when vials of 10,000 units per milliliter instead of 10 units per milliliter were used to flush the infants’ vascular access catheters. This error made national news, which placed a spotlight on the hospital’s process for resolving the error. Fortunately, the infants recovered from the event. This event not only affected California but also had an impact on the nation. To prevent future mistakes, the hospital stopped stocking heparin in pediatric units. Only saline is used to flush vascular access lines (Institute for Safe Medication Practices, 2007).
In addition, HRO theory suggests that HROs have an optimistic attitude and focus on internal organizational practices and culture. There is a fundamental belief that reliability is enhanced by rules and standards of practice, technical and social redundancies, teaching, and decision-making that migrates toward expertise (Chassin, 2012).
The history and background of the HRO paradigm
The initial concept of the HRO paradigm was introduced by a group of researchers at the University of California Berkeley: Todd La Porte, Gene Rochlin, and Karlene Roberts. These researchers examined the links among aircraft carriers, air traffic control, and nuclear power operations (Rochlin, La Porte, and Roberts, 1987; Weick, 1987). Their research found that these industries had similar characteristics, that errors could be minimized through education, and that failures could be avoided by implementing a process to manage complex work and technologies (Rochlin et al., 1987; Weick, 1987).
According to Chassin and Loeb (2013), high reliability science is the study of “organizations in industries like commercial aviation and nuclear power that operate under hazardous conditions while maintaining safety levels that are better than in healthcare” (p. 459). HROs seek to improve reliability and intervene to prevent errors and failures as well as to cope and recover quickly should errors become manifest (Sutcliffe, 2011). HROs are distinguished by their effective management of innately risky technologies through organizational control of both hazards and probability. The hallmark of an HRO is not that it is error-free, but that errors do not disable it. HROs proactively identify weaknesses in the system and use robust process-improvement strategies to address them. They design their reward and incentive systems to recognize the costs of failures as well as the benefits of reliability. They train their people to look for abnormalities, recognize gaps, and act. Their communication consistently shares the big picture of what the organization seeks to do. An important goal is to communicate across the organization in such a way that individuals understand how they fit into the big picture (Chassin and Loeb, 2013).
HRO principles
HROs are unique in their ability both to prevent mishaps and to manage them before they spread throughout the system, thus causing widespread failure. To achieve an HRO environment, an organization must master five principles. As shown in Table 1.2, these principles focus on the practices embedded in the entire organization.
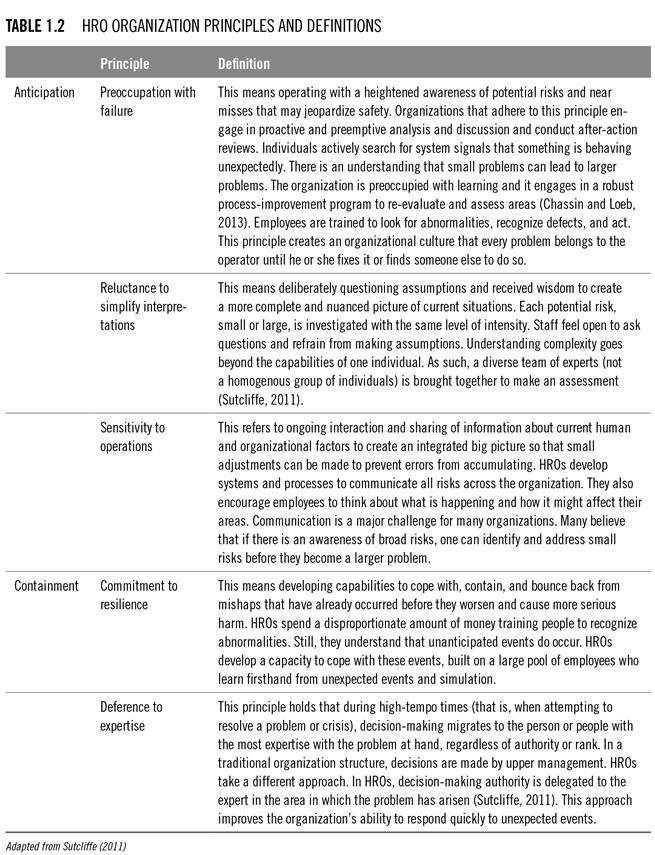
To support the five HRO principles, organizations must adopt a fundamental approach in how they communicate and how individuals interact. That means ensuring the following (Chassin, 2012; Chassin and Loeb, 2013; DuPree, 2014):
When employees feel safe, they will be more likely to report concerns and near misses.
The introduction of HRO as a new paradigm
Human errors are inevitable and are caused by complex factors. Accepting this allows for strategies that can positively affect decision-making and help individuals develop a clearer perception of risks. Ignoring the inevitability of human error will result in continual frustration over adverse events, poor performance, and reactionary measures that focus too heavily on the last person involved in the error. The focus should be on the cumulative effects of organizational breakdowns, flawed defenses, and system failures that allowed the event to occur (Birk, 2015).
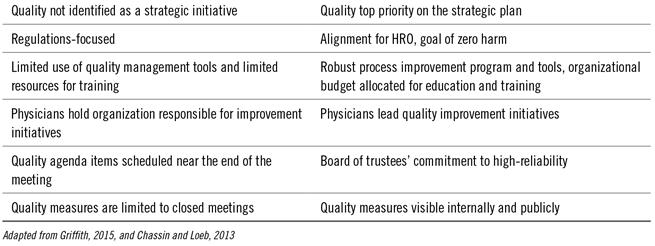
Table 1.3 displays some areas where the healthcare industry is moving from an old paradigm to a new one that focuses on high reliability. Healthcare providers and organizations will need to become comfortable with the new pay-for-performance models and must lead change in the area of transparency. The number of reportable quality outcomes, which consumers and insurance payers use to make decisions regarding healthcare services, is growing. Private organizations such as U.S. News and World Report (2015), Healthgrades (2015), and the Leapfrog Group (2012) also rank hospitals and quality care outcomes.
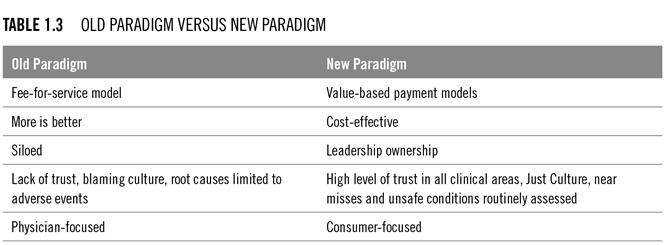
There has been a shift from the perspective that more is better to the perspective that focuses on what is provided given the cost of care. Since the passing of the ACA, more accountability is placed on consumers to secure health insurance. Due to the various options and out-of-pocket expenses, consumers are pausing to evaluate the cost of healthcare. Healthcare systems and hospitals are responding to the consumers’ need to understand the value of their healthcare experience by posting quality outcomes and the cost of procedures on their websites.
Healthcare systems and hospitals are redirecting their focus toward the needs of the consumers. There is growing evidence that partnering with consumers can lead to improvements in quality, outcomes, and cost-effectiveness. Consumers are those individuals who autonomously make decisions regarding their health (Mittler, Martsolf, Telenko, and Scanlon, 2013). They no longer make decisions merely on the word of their physician. Some consumers do their homework and actively participate with their physicians to make healthcare decisions.
Leaders play a role here. To create a culture of safety that focuses on managing risk, increased engagement by leaders is critical (Sutcliffe, 2011). Leaders must commit to creating an environment that encourages team members to speak up. Leaders must also be willing to provide the resources to create a culture of ongoing learning. In the HRO paradigm, quality is a top priority of the healthcare system and hospital’s strategic plan. This occurs when:
- Measures are aligned with the performance goals of all staff.
- There is a commitment to zero-harm goal, starting with the board of trustees.
- There is full engagement with physicians.
- The organizational budget includes resources to provide ongoing education, training, and quality-management tools, which are used for improvement and to redesign care processes (Chassin and Loeb, 2013).
Application to healthcare
HROs have demonstrated success in minimizing errors by creating mindful environments where employees are trained to look for and report small problems that could lead to big ones. They view these small errors and close calls as learning opportunities; they correct them and share details about them across the organization (Chassin, 2012; Shabot, 2015). For the healthcare industry to make real progress in developing HROs, three things must occur:
- The leadership team must commit to a goal of zero harm: If a healthcare organization wants the staff to follow HRO practices, it must start at the top. There must be alignment among the board of trustees, physicians, senior leaders, and department managers, all committed to completely eliminating patient harm.
- HRO principles must be integrated with the organization to develop a culture of safety: Hospitals struggle with this the most. In 2009, The Joint Commission required hospitals to create a culture of safety. Although most healthcare systems hospitals have elected to perform annual safety culture surveys, they have not put much effort or resources toward making sustainable changes to strengthen the culture of safety.
- The organization must adopt a robust process improvement program to improve its quality of care and outcomes: HROs do not specify which process improvement tools and methods to use, but change-management tools, Lean, and Six Sigma are the most widely used. These types of tools incorporate a systematic approach, eliminate waste in the process, and foster discipline in measuring outcomes (Chassin and Loeb, 2013; Sutcliffe, 2011).
Why are HROs needed?
There is overwhelming evidence that preventable patient harm and adverse events continue to occur in U.S. healthcare systems and hospitals. Trends in healthcare outcomes demonstrate that our healthcare system is struggling to deliver consistent and reliable quality care. The dynamics of healthcare are ever-changing, and the pace of this change has made the healthcare industry more difficult for consumers to understand and navigate. Healthcare providers and caregivers work in a complex system with many competing priorities and shrinking revenues. It is as if they are standing on two floating logs—one representing the fee-for-service environment and the other the value-based payment environment. Both of these environments require dedication and focus to be successful. As a result, less attention is directed toward creating HRO environments to drive quality, safety, and service.
Healthcare systems and hospitals have not established sustainable solutions to prevent patients from receiving hospital-acquired infections (HAIs). In 2011, the CDC reported that one in 25 patients in acute care hospitals in the U.S. experienced at least one HAI—an estimate of 772,000 total (2015). Worse, approximately 75,000 patients with HAIs died during their hospitalization. Medical errors are a major killer in the U.S., third only to heart disease and cancer, claiming more than 400,000 lives (James, 2013).
In addition to HAIs, there are other preventable risks in the healthcare environment that could be improved by the adoption of HRO principles. For example, healthcare workers routinely face serious safety and health hazards in the workplace. These hazards may include blood-borne pathogens, biological hazards, chemical and drug exposures, ergonomic hazards from lifting patients, and workplace violence, to name a few (Occupational Safety and Health Administration, 2015). According to the Bureau of Labor Statistics, in 2011, there were more injury and illness cases in healthcare than in any other industry (2014).
Benefits to patient outcomes, financials, safety, and the work environment
In the healthcare industry, the benefits of integrating HRO principles and practices are significant. HRO phenomena are mainly present in large systems that would benefit greatly from anticipating unexpected events to prevent large system failures (La Porte, 1996). Equally, healthcare systems and hospitals have the potential risk of experiencing large system failures. These risks may include financial and human loss, negative impact on the workforce, or a loss of confidence and trust among members of the community, which could have a devastating effect on any health system or hospital.
In embracing HRO practices, health systems and hospitals gain a culture with a strong sense of mission and commitment to reliability in operations and capacity. Organizations that have adopted HRO practices have seen improvement in organizational effectiveness, efficiency, and culture, as well as in customer satisfaction and documentation (The Joint Commission Center for Transforming Healthcare, 2015). Such organizations foster and value safety, quality, and management accountability. They also gain a workforce that is highly skilled, knowledgeable, and engaged in the solutions to make their practice and organization safe (Shabot, 2015). There is also benefit on the cost side. The U.S. spends significant amounts of money on treating HAIs and unnecessary procedures and diagnostic tests.
Between 2010 and 2013, a 9% decline in HAIs saved $12 billion in healthcare costs (CDC, 2015). A further decline in HAI incidence would have a positive financial impact on the healthcare budget, to be reallocated to health programs. As well, a collaborative environment and reward and recognition programs, which are both needed for HRO environments to be successful, could have a positive impact on the work environment and employee turnover. Nurses thrive in environments that provide autonomy and allow for their empowerment, that offer a supportive leadership team, and that promote collegial relationships with their team, and evidence shows that satisfied nurses can have a positive impact on patient outcomes (Twigg and McCullough, 2014).
Summary
The current healthcare system is complex and is burdened with inefficiencies. Overwhelming economic and quality barriers hinder progress in improving quality, safety, and service. The dynamics of the healthcare system are shifting such that HRO is a viable approach to creating a reliable healthcare system for providers, caregivers, and consumers. Evidence suggests that HRO principles create environments that are mindful of anticipating unexpected events and resilient in responding quickly to minimize exposure. In addition, the use of incident reviews in HROs builds institutional knowledge.
Many organizations outside of healthcare have achieved HRO status and have sustained their results over long periods of time (Chassin and Loeb, 2011). Although many healthcare organizations are on the path to adopting HRO principles—and an elite few are close to becoming HROs—we know for sure that the road to an HRO starts and ends with leadership.
Key points
- The current healthcare culture and trends demand a highly reliable healthcare delivery system.
- Adverse events have significant human and economic costs.
- High reliability organizations (HROs) create a culture of safety and help employees to remain alert for the smallest signal of a risk to the organization.
- Healthcare systems and hospitals that anticipate risks and manage unexpected events create a sustainable culture of safety.
- Leaders can build a set of capabilities to respond to adverse events and foster organizational learning.
- Only leaders can build a Just Culture that counteracts the blame game.
- A robust process improvement approach—a combination of Lean, Six Sigma, and change-management tools—is foundational to creating an HRO.
Highly reliable organizations view culture as a core value.
Chapter author:
Cynthia R. Latney, MSN, RN, NE-BC, is chief nursing officer and vice president of patient care services for Penrose St. Francis Health Services in Colorado Springs, Colorado.
Book authors:
Cynthia A. Oster, PhD, MBA, APRN, ACNS-BC, ANP, is nurse scientist for Centura Health and clinical nurse specialist for critical care and cardiovascular services at Porter Adventist Hospital in Denver, Colorado.
Jane S. Braaten, PhD, APRN, CNS, ANP, CPPS, is patient safety manager and nurse scientist at Centura Health, Castle Rock Adventist Hospital in Castle Rock, Colorado.
Information on purchasing High Reliability Organizations: A Healthcare Handbook for Patient Safety & Quality
References
Barton, P. L. (2009). Understanding the U.S. health services system (4th ed.). Chicago, IL: Health Administration Press.
Birk, S. (2015). Accelerating the adoption of a safety culture. The Joint Commission. Retrieved from http://www.jointcommission.org/assets/1/18/
Healthcare_Executive_McKee_032015.pdf
Bureau of Labor Statistics. (2014). Employer-reported workplace injuries and illness. Retrieved from http://www.bls.gov/news.release/pdf/osh.pdf
Center for Patient Safety. (2015). Just culture. Retrieved from http://www.centerforpatientsafety.org/just-culture/
Centers for Disease Control and Prevention. (2015). Chronic diseases: The leading causes of death and disability in the United States. Retrieved from http://www.cdc.gov/chronicdisease/overview/index.htm
Centers for Medicare & Medicaid Services. (2011). Hospital valued-based purchasing program. Retrieved from https://www.cms.gov/Outreach-and-
Education/Medicare-Learning-Network-MLN/MLNProducts/
downloads/Hospital_VBPurchasing_Fact_Sheet_ICN907664.pdf
Centers for Medicare & Medicaid Services. (2015a). Hospital value-based purchasing. Retrieved from https://www.cms.gov/Medicare/Quality-
Initiatives-Patient-Assessment-Instruments/hospital-
value-based-purchasing/index.html?redirect=/
hospital-value-based-purchasing/
Centers for Medicare & Medicaid Services. (2015b). Fiscal year (2016) results for CMS value-based purchasing program. Retrieved from https://www.cms.gov/Newsroom/MediaReleaseDatabase/
Fact-sheets/2015-Fact-sheets-items/2015-10-26.html
Chassin, M. R. (2012). Health care and high reliability: A cautionary tale. 5th International HRO conference. Chicago, IL.
Chassin, M. R. (2015). High reliability in healthcare: Working toward zero harm. Retrieved from http://arabhealthmagazine.com/press-releases/2015/
issue-4/high-reliability-in-healthcare-working-toward-zero-harm/
Chassin, M. R., and Loeb, J. M. (2011). The ongoing quality improvement journey: Next stop, high reliability. Health Affairs, 30(4), pp. 559–568.
Chassin, M. R., and Loeb, J. M. (2013). High-reliability health care: Getting there from here. The Milbank Quarterly. Retrieved from http://www.jointcommission.org/assets/
1/6/Chassin_and_Loeb_0913_final.pdf
Congressional Budget Office. (2015). Budget and economic outlook 2015–2025. Retrieved from https://www.cbo.gov/publication/49892
Covey, S. (1989). The 7 habits of highly effective people: Restoring the character ethic. New York, NY: Simon & Schuster.
DuPree, E. S. (2014). Leading change: The high reliability journey. Hospital Executive Briefing. The Joint Commission. Retrieved from http://www.mha.org/keystone_center/symposium/2015/
documents/using_high_reliability_to_improve_quality.pdf
DuPree, E., Martin, L., Anderson, R., Kathuria, N., Reich, D., Porter, C., and Chassin, M. R. (2009). Improving patient satisfaction with pain management using Six Sigma tools. Joint Commission Journal on Quality and Patient Safety, 35(7), pp. 343–350.
Field, R. I. (2008). Why is health care regulation so complex? Pharmacy and Therapeutics, 33(10), pp. 607–608.
Griffith, J. R. (2015). Understanding high-reliability organizations: Are Baldrige recipients models? Journal of Healthcare Management, 60(1), pp. 44–61.
Healthgrades. (2015). About us. Retrieved from http://www.healthgrades.com
Institute for Safe Medication Practices. (2007). Another heparin error: Learning from mistakes so we don’t repeat them. Retrieved from https://www.ismp.org/newsletters/acutecare/articles/20071129.asp
Institute of Medicine. (1999). To err is human. Retrieved from http://iom.nationalacademies.org/Reports/1999/
To-Err-is-Human-Building-A-Safer-Health-System.aspx
Institute of Medicine. (2011). The Richard and Hinda Rosenthel lecture 2011: New frontiers in patient safety. Retrieved from http://iom.nationalacademies.org/reports/2011/
the-richard-and-hinda-rosenthal-lecture-2011
-new-frontiers-in-patient-safety.aspx
Institute of Medicine. (2013). Best care at lower cost: The path to continuously learning health care in America. Retrieved from http://www.nap.edu/catalog/13444/best-care-at-lower-cost-
the-path-to-continuously-learning
James, J. T. (2013). A new evidence-based element of patient harm associated with hospital care. Journal of Patient Safety, 9(3), pp. 122–128.
The Joint Commission. (2015a). Sentinel event data 1995–3Q 2015. Retrieved from http://www.jointcommission.org/assets/1/18/
General-Information_1995-3Q-2015.pdf
The Joint Commission. (2015b). About the joint commission. Retrieved from http://www.jointcommission.org/about_us/
about_the_joint_commission_main.aspx
The Joint Commission Center for Transforming Healthcare. (2015). High reliability: The gold standard in health care. Retrieved from http://www.centerfortransforminghealthcare.org/hro_portal_main.aspx
Kannampallil, T. G., Schauer, G. F., Cohen, T., and Patel, V. L. (2011). Considering complexity in healthcare systems. Journal of Biomedical Informatics, 44(6), 943–947.
Keckly, P. H., and Coughlin, S. (2012). 2012 survey of U.S. health care consumers: Five-year look back. Washington, DC: Deloitte University Press.
Khatri, N., Brown, G. D., and Hicks, L. L. (2009). From a blame culture to a just culture in health care. Healthcare Management Review, 34 (4), pp. 312–322.
La Porte, T. R. (1996). High reliability organizations: Unlikely, demanding and at risk. Journal of Contingencies and Crisis Management, 4(2), pp. 60–71.
The Leapfrog Group. (2012). How safe is your hospital? Retrieved from http://www.leapfroggroup.org/policy_leadership/leapfrog_news/4894464
LBJ Presidential Library. (2012). The 1965 Medicare amendment to the Social Security Act. Retrieved from http://www.lbjlibrary.org/press/
the-1965-medicare-amendment-to-the-social-security-act
Lipsitz, L. (2012). Understanding health care as a complex system: The foundation for unintended consequences. Journal of American Medical Association, 308(3), pp. 243–244.
Mittler, J. N., Martsolf, G. R., Telenko, S. J., and Scanlon, D. P. (2013). Making sense of “consumer engagement” initiatives to improve health and health care: A conceptual framework guide policy and practice. The Milbank Quarterly, 91(1), pp. 37–77.
Nolan, T., Resar, R., Haraden, C., and Griffin, F. A. (2004). Improving the reliability of health care. IHI Innovation Series white paper. Boston, MA: Institute for Healthcare Improvement. Retrieved from http://www.ihi.org/resources/Pages/IHIWhitePapers/
ImprovingtheReliabilityofHealthCare.aspx
Occupational Safety and Health Administration. (2015). Workplace violence. Retrieved from http://www.osha.gov
Perrow, C. (1999). Normal accidents: Living with high-risk technologies. (2nd ed.). Princeton, NJ: Princeton University Press.
Provera, B., Montefusco, A., and Canato, A. (2010). A “no blame” approach to organizational learning. British Journal of Management, 21(4), pp. 1057–1074.
Rice, T., Unruh, L. Y., Rosenau, P., Barnes, A. J., Saltman, R. B., and van Ginneken, E. (2014). Challenges facing the United States of America in implementing universal coverage. Bulletin of the World Health Organization. Retrieved from http://www.who.int/bulletin/volumes/92/12/14-141762/en/
Roberts, K. H., Bea, R., and Bartles, D. L. (2001). Must accidents happen? Lessons from high-reliability organizations. Academy of Management Perspectives, 15(3), pp. 70–78.
Rochlin, G. I., La Porte, T. R., and Roberts, K. H. (1987). The self-designing high-reliability organization: Aircraft carrier flight operations at sea. Naval War College Review, 40(4), pp. 76–90.
Schumock, G. T., Li, E. C., Suda, K. J., Matusiak, L. M., Hunkler, R. J., Vermeulen, L. C., and Hoffman, J. M. (2014). National trends in prescription drug expenditures and projections for 2014. American Journal of Health-System Pharmacy, 71(6), pp. 482–499.
Shabot, M. M. (2015). New tools for high reliability healthcare. BMJ Quality and Safety, 24(7), pp. 423–424.
Stewart, A. (2011). Risk management: The reactive versus proactive struggle. Journal of Nursing Law, 14(3), pp. 91–95.
Sutcliffe, K. M. (2011). High reliability organizations (HROs). Best Practice & Research Clinical Anaesthesiology, 25(2), pp. 133–144.
Twigg, D., and McCullough, K. (2014). Nurse retention: A review of strategies to create and enhance positive practice environments in clinical settings. International Journal of Nursing Studies, 51(1), pp. 85–92.
U.S. Census Bureau. (2015). Annual and quarterly services. Retrieved from https://www.census.gov/services/index.html
U.S. Department of Health and Human Services. (2014). Key features of the Affordable Care Act. Retrieved from http://www.hhs.gov/healthcare/
facts-and-features/key-features-of-aca/index.html
U.S. News and World Report. (2015). Best hospitals. Retrieved from http://health.usnews.com/best-hospitals
Vogus, T. J., Sutcliffe, K. M., and Weick, K. E. (2010). Doing no harm: Enabling, enacting, and elaborating a culture of safety. Academy of Management Perspectives, 24(6), pp. 60–77.
Wagner, K. (2014). Health care reform and leadership: Switching from volume to value. Physician Leadership Journal, 1(1), pp. 22–26.
Weick, K. E. (1987). Organizational culture as a source of high reliability. California Management Review, 29(2), pp. 112–127.
Weick, K. E., and Sutcliffe, K. M. (2001). Managing the unexpected: Assuring high performance in an age of complexity. San Francisco, CA: Jossey-Bass.
Weick, K. E., and Sutcliffe, K. M. (2006). Mindfulness and the quality of organizational attention. Organization Science, 17(4), pp. 514–524.
Weick, K. E., and Sutcliffe, K. M. (2007). Managing the unexpected: Resilient performance in an age of uncertainty (2nd ed.). San Francisco, CA: Jossey-Bass.
Wildavsky, A. B. (1988). Searching for safety. Piscataway, NJ: Transaction Publishers.
Wilson, K. A., Burke, C. S., Priest, H. A., and Salas, E. (2005). Promoting healthcare safety through training high reliability teams. Quality & Safety in Healthcare, 14(4), pp. 303–309.
World Health Organization. (2015). World health statistics 2014. Retrieved from http://www.who.int/mediacentre/news/releases/
2014/world-health-statistics-2014/en/