This chapter from Implementing the Evidence-Based Practice (EBP) Competencies in Healthcare explains how evidence-based practice improves healthcare quality and patient outcomes while reducing costs and discusses multiple barriers to EBP that persist in healthcare settings.
"To know and not to do is really not to know."
–Stephen R. Covey
Setting the stage
 Have you ever wondered why the United States spends more money on healthcare than any western country, yet it ranks 37th in world health outcomes? Have you ever questioned why patients are awakened every 2 to 4 hours for vital signs in the hospital when they are stable and in desperate need of sleep? Or wondered why nurses work 12-hour shifts when research shows the multiple adverse outcomes of working lengthy hours for both clinicians and patients? Have you ever thought about the millions of healthcare dollars that could be saved if all primary care providers would follow the evidence-based recommendations of the U.S. Preventive Services Task Force? Have you ever questioned why it often takes decades for the evidence that is generated from research to be translated into the real world to improve healthcare quality and patient outcomes?
Have you ever wondered why the United States spends more money on healthcare than any western country, yet it ranks 37th in world health outcomes? Have you ever questioned why patients are awakened every 2 to 4 hours for vital signs in the hospital when they are stable and in desperate need of sleep? Or wondered why nurses work 12-hour shifts when research shows the multiple adverse outcomes of working lengthy hours for both clinicians and patients? Have you ever thought about the millions of healthcare dollars that could be saved if all primary care providers would follow the evidence-based recommendations of the U.S. Preventive Services Task Force? Have you ever questioned why it often takes decades for the evidence that is generated from research to be translated into the real world to improve healthcare quality and patient outcomes?
Tina Magers (nursing professional development and research coordinator at Mississippi Baptist Health Systems) and her team wondered why catheter-associated
urinary tract infections (CAUTIs) affect as many as 25% of all hospitalized patients and questioned what evidence exists that could inform a practice
change to reduce these infections in their hospital. (This is Step #0 in the seven-step evidence-based practice [EBP] process, which we describe in detail
later in this chapter.) As a result, the team formed the following question in a format called PICOT (Patient population, Intervention or Interest area,
Comparison intervention or group, Outcome, and Time; Step #1 in EBP) that facilitated them to conduct an expedited effective search for the best evidence
(Magers, 2015):
In adult patients hospitalized in a long-term acute care hospital (P), how does the use of a nurse-driven protocol for evaluating the appropriateness
of short-term urinary catheter continuation or removal (I) compared to no protocol (C) affect the number of catheter days and CAUTI rates (O) over a
six-month post-intervention period (T)?
The team conducted an evidence search to answer this clinical question using the Cumulative Index to Nursing and Allied Health Literature (CINAHL), the
Cochrane Database of Systematic Reviews, Cochrane Central Register of Controlled Trials, the Database of Abstracts of Reviews of Effects (DARE), Ovid
Clinical Queries, and PubMed (Step #2 in EBP), followed by rapid critical appraisal of 15 studies found in the search (Step #3 in EBP). A synthesis of the
15 studies led the team to conclude that early removal of urinary catheters would likely reduce catheter days and CAUTIs (the identified outcomes).
Therefore, the team wrote a protocol based on the evidence, listing eight criteria for the continuation of a short-term urinary catheter (Step #4 in EBP).
After the protocol was presented to the medical executive committee at their hospital for approval, a process for the change was put into practice,
including an education plan with an algorithm that was implemented in small group inservices for the nurses, posters, and written handouts for physicians.
An outcomes evaluation (Step #5 in the EBP process) revealed a significant reduction in catheter days and a clinically significant reduction of 33% in
CAUTIs. The team disseminated the outcomes of the project to internal audiences (e.g., their Nursing Quality Council, the EBP and Research Council, Nursing
Leadership Council, Organization Infection Control Committee) and external venues (presentations at regional conferences and a publication in the American Journal of Nursing) (Magers, 2013). (Step #6 in the EBP process.)
This is a stellar exemplar of how a team with a spirit of inquiry and a commitment to improving healthcare quality can use the seven-step EBP process
discussed in this chapter to improve patient outcomes and reduce hospital costs.
Evidence-based practice and the quadruple aim in healthcare
Findings from an extensive body of research support that EBP improves the quality and safety of healthcare, enhances health outcomes, decreases geographic
variation in care, and reduces costs (McGinty & Anderson, 2008; Melnyk & Fineout-Overholt, 2015; Melnyk, Fineout-Overholt, Gallagher-Ford, &
Kaplan, 2012a). In the United States, EBP has been recognized as a key factor in meeting the Triple Aim in healthcare, defined as (Berwick, Nolan, &
Whittington, 2008):
- Improving the patient experience of care (including quality and satisfaction)
- Improving the health of populations
- Reducing the per capita cost of healthcare
The Triple Aim has now been expanded to the Quadruple Aim: the fourth goal being to improve work life and decrease burnout in clinicians (Bodenheimer &
Sinsky, 2014).
Because EBP has been found to empower clinicians and result in higher levels of job satisfaction (Strout, 2005), it also can assist healthcare systems in
achieving the Quadruple Aim. However, regardless of its tremendous positive outcomes, EBP is not standard of care in healthcare systems throughout the
United States or the rest of the world due to multiple barriers that have continued to persist over the past decades. Some of these barriers include
(Melnyk & Fineout-Overholt, 2015; Melnyk et al., 2012a; Melnyk et al., 2012b; Melnyk et al., 2016; Pravikoff, Pierce, & Tanner, 2005; Titler,
2009):
- Inadequate knowledge and skills in EBP by nurses and other healthcare professionals
- Lack of cultures and environments that support EBP
- Misperceptions that EBP takes too much time
- Outdated organizational politics and policies
- Limited resources and tools available for point-of-care providers, including budgetary investment in EBP by chief nurse executives
- Resistance from colleagues, nurse managers, and leaders
- Inadequate numbers of EBP mentors in healthcare systems
- Academic programs that continue to teach baccalaureat, master’s, and doctor of nursing practice students the rigorous process of how to conduct research instead of taking an evidence-based approach to care
Urgent action is needed to rapidly accelerate EBP in order to reduce the tremendously long lag between the generation of research findings and their
implementation in clinical settings. Many interventions or treatments that have been found to improve outcomes through research are not standard of care
throughout healthcare systems or have never been used in clinical settings. It took more than 20 years for neonatal and pediatric intensive care units to
adopt the Creating Opportunities for Parent Empowerment (COPE) Program for parents of preterm infants and critically ill children even though multiple
intervention studies supported that COPE reduced parent depression and anxiety, enhanced parental-infant interaction, and improved child outcomes (Melnyk
& Fineout-Overholt, 2015). It was not until findings from a National Institute of Nursing Research funded randomized controlled trial supported that
COPE reduced neonatal intensive care unit (NICU) length of stay in premature infants by 4 days (8 days in preterms less than 32 weeks) and its associated
substantial decreased costs that NICUs across the country began to implement the intervention as standard of care (Melnyk & Feinstein, 2009; Melnyk et
al., 2006).
If not for an improvement in “so-what” outcomes (outcomes of importance to the healthcare system, such as decreased length of stay and costs), COPE would
not have been translated into NICU settings to improve outcomes in vulnerable children and their families. On the other hand, many interventions or
practices that do not have a solid body of evidence to support them continue to be implemented in healthcare, including double-checking pediatric
medications, assessing nasogastric tube placement with air, and taking vital signs every 2 or 4 hours for hospitalized patients. These practices that are
steeped in tradition instead of based upon the best evidence result in less than optimum care, poor outcomes, and wasteful healthcare spending.
Definition of evidence-based practice
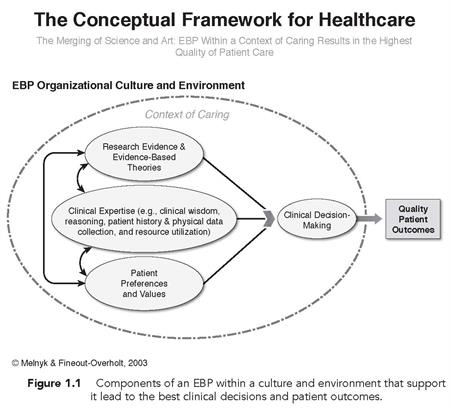
As EBP evolved, it was defined as the conscientious use of current best evidence to make decisions about patient care (Sackett, Straus, Richardson,
Rosenberg, & Haynes, 2000). Since this earlier definition, EBP has been broadened to include a lifelong problem-solving approach to how healthcare is
delivered that integrates the best evidence from high-quality studies with a clinician’s expertise and also a patient’s preferences and values (Melnyk
& Fineout-Overholt, 2015; see Figure 1.1).
Incorporated within a clinician’s expertise are:
- Clinical judgment
- Internal evidence from the patient’s history and physical exam, as well as data gathered from EBP, quality improvement, or outcomes management projects
- An evaluation of available resources required to deliver the best practices
Some barriers inhibit the uptake of EBP across all venues and disciplines within healthcare. Although the strongest level of evidence that guides clinical
practice interventions (i.e., Level I evidence) are systematic reviews of randomized controlled trials followed by well-designed randomized controlled
trials (i.e., Level II evidence), there is a limited number of systematic reviews and intervention studies in the nursing profession. Single descriptive
quantitative and qualitative studies, which are considered lower-level evidence, continue to dominate the field; see Table 1.1 for levels of evidence that
are used to guide clinical interventions.
However, all studies that are relevant to the clinical question should be included in the body of evidence that guides clinical practice. In addition,
clinicians often lack critical appraisal skills needed to determine the quality of evidence that is produced by research. Critical appraisal of evidence is
an essential step in EBP given that strength or level of evidence plus quality of that evidence gives clinicians the confidence to act and change practice.
If Level I evidence is published but is found to lack rigor and be of poor quality through critical appraisal, a clinician would not want to make a
practice change based on that evidence.
 (Click image to enlarge)
(Click image to enlarge)
TABLE 1.1 RATING SYSTEM FOR THE HIERARCHY OF EVIDENCE TO GUIDE CLINICAL INTERVENTIONS
|
Level
|
Explanation
|
|
I
|
Evidence from a systematic review or meta-analysis of all relevant randomized controlled trials (RCTs)
|
|
II
|
Evidence obtained from well-designed RCTs
|
|
III
|
Evidence obtained from well-designed controlled trials without randomization
|
|
IV
|
Evidence from well-designed case-control and cohort studies
|
|
V
|
Evidence from systematic reviews of descriptive and qualitative studies
|
|
VI
|
Evidence from single descriptive or qualitative studies
|
|
VII
|
Evidence from the opinion of authorities and/or reports of expert committees
|
Source: Modified from Elwyn et al. (2015) and Harris et al. (2001)
.
The seven steps of evidence-based practice
Evidence-based practice was originally described as a five-step process including (Sackett et al., 2000):
-
Ask the clinical question in PICOT format.
-
Search for the best evidence.
-
Critically appraise the evidence.
-
Integrate the evidence with a clinician’s expertise and a patient’s preferences and values.
-
Evaluate the outcome of the practice change.
In 2011, Melnyk and Fineout-Overholt added two additional steps to the process, resulting in the following seven-step EBP process (see Table 1.2).
TABLE 1.2
THE SEVEN STEPS OF EVIDENCE-BASED PRACTICE
|
Step
|
Explanation
|
|
0
|
Cultivate a spirit of inquiry within an EBP culture and environment.
|
|
1
|
Ask the burning clinical question in PICOT format.
|
|
2
|
Search for and collect the most relevant best evidence.
|
|
3
|
Critically appraise the evidence (i.e., rapid critical appraisal, evaluation, synthesis, and recommendations).
|
|
4
|
Integrate the best evidence with one’s clinical expertise and patient preferences and values in making a practice decision or change.
|
|
5
|
Evaluate outcomes of the practice decision or change based on evidence.
|
|
6
|
Disseminate the outcomes of the EBP decision or change.
|
Step #0: Cultivate a spirit of inquiry within an EBP culture and environment
The first step in EBP is to cultivate a spirit of inquiry, which is a continual questioning of clinical practices. When delivering care to patients, it is
important to consistently question current practices: For example, is Prozac or Zoloft more effective in treating adolescents with depression? Does use of
bronchodilators with metered dose inhalers (MDIs) and spacers versus nebulizers in the emergency department (ED) with asthmatic children lead to better
oxygenation levels? Does double-checking pediatric medications lead to fewer medication errors?
Cultures and environments that support a spirit of inquiry are more likely to facilitate and sustain a questioning spirit in clinicians. Some key
components of an EBP culture and environment include (Melnyk, 2014; Melnyk & Fineout-Overholt, 2015; Melnyk et al., 2012a, 2016):
-
An organizational vision, mission, and goals that include EBP
-
An infrastructure with EBP tools and resources
-
Orientation sessions for new clinicians that communicate an expectation of delivering evidence-based care and meeting the EBP competencies for
practicing registered nurses (RNs) and advanced practice nurses (APNs)
-
Leaders and managers who “walk the talk” and support their clinicians to deliver evidence-based care
-
A critical mass of EBP mentors to work with point-of-care clinicians in facilitating evidence-based care
-
Evidence-based policies and procedures
-
Orientations and ongoing professional development seminars that provide EBP knowledge and skills-building along with an expectation for EBP
-
Integration of the EBP competencies in performance evaluations and clinical ladders
-
Recognition programs that reward evidence-based care
Step #1: Ask the burning clinical question in PICOT format
After a clinician asks a clinical question, it is important to place that question in PICOT format to facilitate an evidence search that is effective in
getting to the best evidence in an efficient manner. PICOT represents:
-
Sometimes, there is not a time element; therefore you see PICO rather than PICOT.
P: Patient population
-
I: Intervention or Interest area
-
C: Comparison intervention or group
-
O: Outcome
-
T: Time (if relevant)
For example, the clinical questions asked in Step #0 that all involve interventions or treatments should be rephrased in the following PICOT format to
result in the most efficient and effective database searches:
-
In depressed adolescents (P), how does Prozac (I) compared to Zoloft (C) affect depressive symptoms (O) 3 months after starting treatment (T)?
-
In asthmatic children seen in the ED (P), how do bronchodilators delivered with MDIs with spacers (I) compared to nebulizers (C) affect oxygenation
levels (O) 1 hour after treatment (T)?
-
In hospitalized children (P), how does double-checking pediatric medications with a second nurse (I) compared to not double-checking (C) affect
medication errors (O) during a 30-day time period (T)?
In addition to intervention or treatment questions, other types of PICOT questions include meaning questions, diagnosis questions, etiology questions, and
prognosis questions that are addressed in Chapter 3.
Step #2: Search for and collect the most relevant best evidence
After the clinical question is placed in PICOT format with the proper template, each keyword in the PICOT question should be used to systematically search
for the best evidence; this strategy is referred to as keyword searching. For example, to gather the evidence to answer the intervention PICOT
questions in Step #1, you would first search databases for systematic reviews and randomized controlled trials given that they are the strongest levels of
evidence to guide practice decisions.
However, the search should extend to include all evidence that answers the clinical question. Each keyword or phrase from the PICOT question (e.g.,
depressed adolescents, Prozac, Zoloft, depressive symptoms) should be entered individually and searched. Searching controlled vocabulary that matches the
keywords is the next step in a systematic approach to searching.
In the final step, combine each keyword and controlled vocabulary previously searched, which typically yields a small number of studies that should answer
the PICOT question. This systematic approach to searching for evidence typically yields a small number of studies to answer the clinical question versus a
less systematic approach, which usually produces a large number of irrelevant studies. More specific information about searching is covered in Chapter 4.
Step #3: Critically appraise the evidence
After relevant evidence has been found, critical appraisal begins. First, it is important to conduct a rapid critical appraisal (RCA) of each study from
the data search to determine whether they are keeper studies: that is, they indeed answer the clinical question. This process includes answering
the following questions:
- Are the results of the study valid?
Did the researchers use the best methods to conduct the study (study validity)? For example, assessment of a study’s validity determines whether
the methods used to conduct the study were rigorous.
- What are the results?
Do the results matter, and can I get similar results in my practice (study reliability)?
- Will the results help me in caring for my patients?
Is the treatment feasible to use with my patients (study applicability)?
Rapid critical appraisal checklists can assist clinicians in evaluating validity, reliability, and applicability of a study in a time-efficient way. See
Chapter 5 for one example of an RCA checklist for randomized controlled trials and Melnyk & Fineout-Overholt (2015) for a variety of RCA checklists.
After an RCA is completed on each study and found to be a keeper, it is included in the evaluation and synthesis of the body evidence to determine whether
a practice change should be made. Chapter 5 contains more information on critically appraising, evaluating, and synthesizing evidence.
Step #4: Integrate the best evidence with one’s clinical expertise and patient preferences and values in making a practice decision or change
After the body of evidence from the search is critically appraised, evaluated, and synthesized, it should be integrated with a clinician’s expertise and
also a patient’s preferences and values to determine whether the practice change should be conducted. Providing the patient with evidence-based information
and involving him or her in the decision regarding whether he or she should receive a certain intervention is an important step in EBP. To facilitate
greater involvement of patients in making decisions about their care in collaboration with healthcare providers, there has been an accelerated movement in
creating and testing patient-decision support tools, which provide evidence-based information in a relatable understandable format (Elwyn et al., 2015).
Step #5: Evaluate outcomes of the practice decision or change based on evidence
After making a practice change based on the best evidence, it is critical to evaluate outcomes—the consequences of an intervention or treatment. For
example, an outcome of providing a baby with a pacifier might be a decrease in crying. Outcomes evaluation is essential to determine the impact of the
practice changes on healthcare quality and health outcomes. It is important to target “so-what” outcomes that the current healthcare system considers
important, such as complication rates, length of stay, rehospitalization rates, and costs given that hospitals are currently being reimbursed based on
their performance on these outcomes (Melnyk & Morrison-Beedy, 2012). A more thorough discussion of approaches to outcomes evaluation is included in
Chapter 7.
Step #6: Disseminate the outcomes of the EBP decision or change
Silos often exist, even within the same healthcare organization. So that others can benefit from the positive changes resulting from EBP, it is important
to disseminate the findings. Various avenues for dissemination include institutional EBP rounds; poster and podium presentations at local, regional, and
national conferences; and publications. More detailed information about disseminating outcomes of EBP is included in Chapter 9.
Rationale for the new EBP competencies
To accelerate the uptake of EBP and ensure that nurses are competent in the delivery of evidence-based care, a new set of EBP competencies was recently
developed for practicing RNs and APNs. Competencies are typically developed and used to ensure the delivery of high-quality, safe nursing care, which
should be an expectation from the public (American Nurses Association, 2010; Melnyk, Gallagher-Ford, Long, & Fineout-Overholt, 2014). The process of
developing these competencies along with the research conducted to further validate them are described in Chapter 2.
Summary
This chapter discussed how evidence-based practice (EBP) improves healthcare quality, patient outcomes, and cost reductions, yet multiple barriers persist
in healthcare settings that need to be rapidly overcome. Ensuring that clinicians meet the newly established EBP competencies along with creating cultures
and environments that support EBP are key strategies to transform the current state of nursing practice and healthcare delivery to its highest level. This
chapter discussed how evidence-based practice (EBP) improves healthcare quality, patient outcomes, and cost reductions, yet multiple barriers persist in
healthcare settings that need to be rapidly overcome. Ensuring that clinicians meet the newly established EBP competencies along with creating cultures and
environments that support EBP are key strategies to transform the current state of nursing practice and healthcare delivery to its highest level.
Information on purchasing
Implementing the Evidence-Based Practice (EBP) Competencies in Healthcare.
References
American Nurses Association. (2010). Nursing: Scope and standards of practice (2nd edition). Silver Spring, MD: American Nurses Association.
Berwick, D. M., Nolan, T. W., & Whittington, J. (2008). The Triple Aim: Care, health, and cost. Health Affairs, 27(3), 759–769.
Bodenheimer, T., & Sinsky, C. (2014). From Triple to Quadruple Aim: Care of the patient requires care of the provider. Annals of Family Medicine, 12, 573–576.
Elwyn, G., Quinlan, C., Mulley, A., Agoritsas, T., Vandik, P. O., & Guyatt, G. (2015). Trustworthy guidelines—excellent; customized care tools—even
better. BioMed Central Medicine, 13(1), 199. Modified from Guyatt, G., & Rennie, D. (2002), Users’ guides to the medical literature.
Chicago, IL: American Medical Association.
Harris, R. P., Hefland, M., Woolf, S. H., Lohr, K. N., Mulrow, C. D., Teutsch, S. M., & Atkins, D. (2001). Current methods of the U.S. Preventive
Services Task Force: A review of the process. American Journal of Preventive Medicine, 20, 21–35.
Magers, T. (2013). Using evidence-based practice to reduce catheter-associated urinary tract infections. American Journal of Nursing, 113(6),
34–42.
Magers, T. L. (2015). Using evidence-based practice to reduce catheter-associated urinary tract infections in a long-term acute care facility. In B. M.
Melnyk & E. Fineout-Overholt (Eds.), Evidence-based practice in nursing & healthcare. A guide to best practice (3rd ed.) (pp. 70–73).
Philadelphia, PA: Wolters Kluwer.
McGinty, J., & Anderson, G. (2008). Predictors of physician compliance with American Heart Association guidelines for acute myocardial infarction. Critical Care Nursing Quarterly, 31(2), 161–172.
Melnyk, B. M. (2014). Building cultures and environments that facilitate clinician behavior change to evidence-based practice: What works? Worldviews on Evidence-Based Nursing, 11(2), 79–80.
Melnyk, B. M., & Fineout-Overholt, E. (2011). Evidence-based practice in nursing & healthcare. A guide to best practice (pp. 1–24).
Philadelphia, PA: Wolters Kluwer/Lippincott Williams & Wilkins.
Melnyk, B. M., & Fineout-Overholt, E. (2015). Evidence-based practice in nursing & healthcare. A guide to best practice (3rd ed.) (pp.
3–23). Philadelphia, PA: Wolters Kluwer.
Melnyk, B. M., Fineout-Overholt, E., Gallagher-Ford, L., & Kaplan, L. (2012a). The state of evidence-based practice in US nurses: Critical implications
for nurse leaders and educators. Journal of Nursing Administration, 42(9), 410–417.
Melnyk, B. M., Grossman, D., Chou, R., Mabry-Hernandez, I., Nicholson, W., Dewitt, T.G. . . . & Flores, G. (2012b). USPSTF perspective on
evidence-based preventive recommendations for children. Pediatrics, 130(2), e399–e407.
Melnyk, B. M., & Feinstein, N. (2009). Reducing hospital expenditures with the COPE (Creating Opportunities for Parent Empowerment) program for parents
and premature infants: An analysis of direct healthcare neonatal intensive care unit costs and savings. Nursing Administrative Quarterly, 33(1),
32–37.
Melnyk, B. M., Feinstein, N. F., Alpert-Gillis, L., Fairbanks, E., Crean, H. F., Sinkin, R., & Gross, S. J. (2006). Reducing premature infants’ length
of stay and improving parents’ mental health outcomes with the COPE NICU program: A randomized clinical trial. Pediatrics, 118(5), e1414–e1427.
Melnyk, B. M., Gallagher-Ford, L., Thomas, B. K., Troseth, M., Wyngarden, K., & Szalacha, L. (2016). A study of chief nurse executives indicates low
prioritization of evidence-based practice and shortcomings in hospital performance metrics across the United States. Worldviews on Evidence-Based Nursing, 13(1), 6–14.
Melnyk, B. M., Gallagher-Ford, L., Long, L., & Fineout-Overholt, E. (2014). The establishment of evidence-based practice competencies for practicing
nurses and advanced practice nurses in real-world clinical settings: Proficiencies to improve healthcare quality, reliability, patient outcomes, and costs. Worldviews on Evidence-Based Nursing, 11(1), 5–15.
Melnyk, B. M., & Morrison-Beedy, D. (2012). Setting the stage for intervention research: The “so what,” “what exists” and “what’s next” factors. In B.
M. Melnyk & D. Morrison-Beedy (Eds.), Designing, conducting, analyzing and funding intervention research. A practical guide for success (pp.
1–9). New York, NY: Springer Publishing Company.
Pravikoff, D. S., Pierce, S. T., & Tanner A. (2005). Evidence-based practice readiness study supported by academy nursing informatics expert panel. Nursing Outlook, 53(1), 49–50.
Sackett, D. L., Straus, S. E., Richardson, W. S., Rosenberg, W., & Haynes, R. B. (2000). Evidence-based medicine: How to practice and teach EBM. London, UK: Churchill Livingstone.
Strout, T. D. (2005). Curiosity and reflective thinking: Renewal of the spirit. In Clinical scholars at the bedside: An EBP mentorship model for today
[electronic version]. Excellence in Nursing Knowledge. Indianapolis, IN: Sigma Theta Tau International.
Titler, M. G. (2009). Developing an evidence-based practice. In G. LoBiondo-Wood & J. Haber (Eds.), Nursing research: Methods and critical appraisal for evidence-based practice (7th ed.) (pp. 385–437). St Louis, MO: Mosby.
Book authors:
Bernadette Mazurek Melnyk, PhD, RN, CPNP/PMHNP, FAANP, FNAP, FAAN , is associate vice president for health promotion, university chief wellness officer, and professor and dean of the College of Nursing at The Ohio State University. She also is professor of pediatrics and professor of psychiatry at Ohio State’s College of Medicine.
Lynn Gallagher-Ford, PhD, RN, DPFNAP, NE-BC, is director of the Center for Transdisciplinary Evidence-based Practice (CTEP) and clinical associate professor in the College of Nursing at The Ohio State University.
Ellen Fineout-Overholt, PhD, RN, FNAP, FAAN, is the Mary Coulter Dowdy Distinguished Nursing Professor in the College of Nursing & Health Sciences at the University of Texas at Tyler.