On Monday, 17 February, 13 people who tested positive or had a high likelihood of testing positive for novel coronavirus (COVID-19)
arrived in Nebraska. They’d been among the 328 US passengers aboard the Diamond Princess cruise ship docked in Yokohama, Japan. After a stop in California, the 13 were flown to the National Quarantine Unit at the University of Nebraska Medical Center. One patient with a chronic condition was admitted to our Biocontainment Unit, the largest in the nation, where we cared for Ebola patients in 2014.
The coronavirus outbreak is rapidly evolving—and it presents special risks for frontline healthcare professionals. Although stats are constantly in flux, in mid-February,
CNN reported that over 1,700 frontline medics had been infected with the coronavirus in China, and six had died.
Let’s be ready
Quarantine measures are working to slow the spread of the illness, but the ease of international travel creates challenges worldwide. We should always be prepared to protect ourselves. The best way to do that is to ask questions now—wherever you work and care for patients. Know the process and protocols for managing infection control and respiratory protection programs within your facility, and make sure others do as well. Review checklists and restock supply cabinets.
It’s equally important to brush up on your emergency preparedness and isolation skills. Caring for patients with infectious diseases is different than it used to be because every day organisms are becoming more resistant to our antibiotics and other therapies. Transmission of these diseases has not changed, and we have good processes to stay safe.
The Centers for Disease Control and Prevention and
World Health Organization websites offer resources that can help.
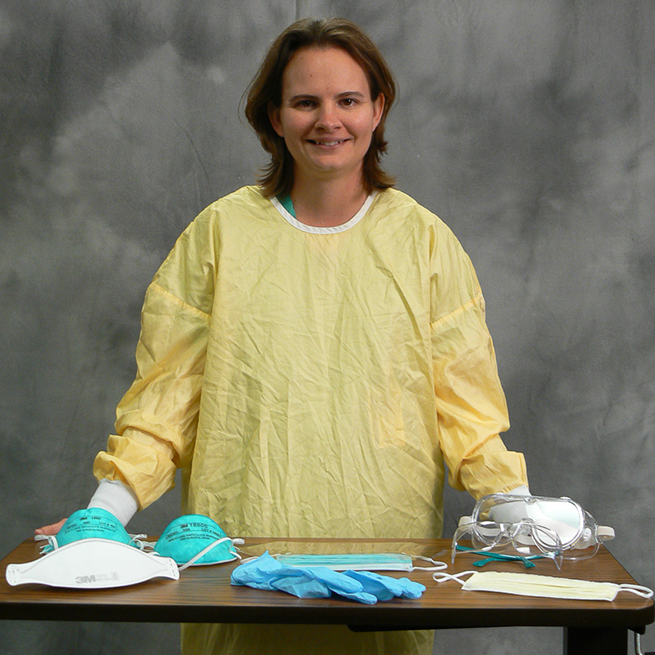
The University of Nebraska Medical Center is here to help, too. Through our HEROES (Healthcare and Emergency Responder Organization Education through Simulation) program at the UNMC College of Nursing, my team and I have been helping clinicians prepare for emergency situations since 2005.
Our training videos and guidelines demonstrate how to, for example, properly wear personal protective equipment (PPE), especially N95 respirators. When they’re caring for patients with infectious disease, knowing
the right way to don and doff a respirator is crucial to keeping clinicians safe.
Our original hospital
PPE video, recorded in 2009, has received nearly 400,000 views on YouTube. During the reemergence of Ebola in 2019, the WHO reached out to ask about using our training materials. We make it easy for anyone to download video files and other educational content at
www.unmcheroes.org so institutions can track usage in their learning management systems. I encourage you to make use of these tools.
Mindfulness matters
My focus on the protective power of PPE began when I worked as a nurse myself and felt uncomfortable donning and doffing my own respirator. My mentor, Shawn Gibbs, PhD, CIH, who had experience in public health and industrial hygiene, knew the science behind what makes respirators work. He talked about how particles were drawn into the material and the importance of seal and exactly where the straps are placed. He also reminded me that a simple patient care mask is a powerful tool. I learned that putting a mask on a coughing patient and a mask on myself as the caregiver was a simple way to keep both of us safe.
That’s when my passion for PPE was born. I had identified something that wasn’t comfortable for me as a nurse and found someone who needed a voice to connect with healthcare workers. The experience inspired me to make more connections to improve things for all nurses. Nurses who feel safe will stay at the bedside longer.
As the coronavirus crisis evolves, it’s easy to feel swept up in the panic. Yet, as nurses and nursing leaders, it’s our job to consistently remain mindful—to slow down and think about what we’ve done, what we’ve touched. We should always be assessing risk in our environment.
When dealing with infection control, proper safety behaviors can keep us safe. Early pilot research we’ve done at UNMC shows there are still gaps in safety when it comes to PPE.
Nursing schools don’t always focus on training students how to use respirators, since many aren’t likely to encounter airborne isolation patients in their clinical rotations. Hospital employees may be fit-tested but may not be given guidance on how to don and doff beyond what’s on the product packaging.
We’ve learned through our pilot studies that people often think they’re better at donning and doffing respirators than they actually are. They may not be sure where to place the straps of the respirator—the top strap on the top of the head and the bottom strap against the skin of the neck. Grooming and hairstyles also can affect safety. Loose hairstyles can impact control during the doffing process, which is critical to safety. In order for a respirator to seal properly, the face must be clean shaven every day, especially where the respirator touches the face.
Another thing our pilot studies have shown: People did a better job learning the right way to don and doff a respirator after they watched and rated a video of their own performance. Seeing themselves and reflecting led to lasting improvement in behaviors.
That’s inspiring. It shows that technology such as video can be used in new ways to make learning more engaging. That’s important to us at HEROES. We were one of the first programs to use nursing simulators for emergency preparedness education, and HEROES is currently experimenting with using virtual reality as a teaching tool for concepts like triage. The basics work well, too. Our robust web and social media presence have helped us share our educational materials with healthcare facilities throughout our state—as well as across the world.
Safe for the future
Knowing we can protect ourselves makes us feel safe. Improving that sensation of safety for nurses at the bedside has a profound impact—on patient care, on nurses’ health, and even on the nursing profession.
The situation with the coronavirus is unpredictable—as is the case with all outbreaks. This occurrence may not end up being a true threat in all areas of the world. It may never arrive in your town or at your facility. Yet COVID-19 is a reminder of the importance of being ready. There’s no doubt we’ll encounter new and different outbreaks in the future. Although we can’t predict when or where they’ll occur, we can be sure that, as nurses on the frontlines of care, we’re armed with the knowhow to keep our patients—and ourselves—safe.
Beth Beam, PhD, RN, is the Assistant Professor and Program Director for the University of Nebraska Medical Center College of Nursing’s HEROES program, which provides education and training to prepare healthcare workers and healthcare professions students for emergencies. She is a member of Sigma’s Gamma Pi at-Large Chapter in Nebraska, USA.